Reducing the Stigma of Maternal Mental Health Disorders
Advocates are hopeful that by normalizing the prevalence of Perinatal Mood and Anxiety Disorders (PMADs), more women will understand the differences between the baby blues and postpartum depression. Greater awareness will allow for the realization that “something’s not right”— with me, my wife, my sister, my daughter, and thus more screenings for prenatal and postpartum depression and anxiety. PMADs are very treatable with professional help. With help you will feel better.
May is Maternal Mental Health Awareness Month. It’s a month to raise awareness for postpartum depression and anxiety and just how prevalent it is—One in seven! It’s a month to educate people about postpartum PTSD and that you CAN in fact be traumatized by your birth. It’s also an opportunity to let our community know that some women are at a higher risk for developing postpartum psychosis (a personal or family history of bipolar disorder increases her risk). Many are surprised to know that up to 80% of new moms experience the baby blues, it’s that common! Perinatal Mood and Anxiety Disorders (PMADs) are the number one complication of pregnancy.
Advocates are hopeful that by normalizing the prevalence of maternal mental health disorders, more women will understand the differences between the baby blues and postpartum depression. Greater awareness will help people detect when “something’s not right”— with me, my wife, my sister, my daughter, and hopefully lead to more screenings for prenatal and postpartum depression and anxiety. It's estimated that less than 50% of women struggling with a PMAD seek treatment, despite the fact that they're extremely treatable with professional help. Some reports estimate as few as 15% of women who struggle seek treatment, though it's difficult to know for sure since shame and stigma prevent many from reaching out.
There are many ways to support the mental health of women and their families during the childbearing years. Below are 5 ways that you can help reduce the stigma of maternal mental health disorders and advocate for greater awareness in our community.
5 Ways to Advocate for Maternal Mental Health
- Join your local chapter of Postpartum Support International. In San Diego, our chapter is called the Postpartum Health Alliance. I’m proud to volunteer my time as the Outreach Co-Chair and serve as a warmline volunteer. There are loads of ways to help build awareness and educate your community through your local organization.
- Display a Blue Dot—the new national symbol for Maternal Mental Health. You can purchase your magnet or sticker here. Not only are you supporting this important cause with your financial contribution, but you’re letting those around you know that you’re an aware and concerned citizen; It’s a conversation starter that will let more people know about PMADS and the risks to moms and babies who go untreated.
- Write letters to congress in support of the Bringing Postpartum Depression Out of the Shadows Act of 2015! That will provide grants for screening and treatment for perinatal mood and anxiety disorders.
- Participate in your local Climb Out of the Darkness hike in June to raise awareness of maternal mental health disorders. These events are coordinated by local volunteers through Postpartum Progress. To join San Diego’s hike, contact Julie Thorpe
- Don’t forget to ask the mothers you love and care for about their mental health: How are you sleeping? How are you eating? How are you feeling? If you're not sure how to address someone you think is struggling, this article provides some helpful strategies.
If you suspect that you or someone you love has a perinatal mood or anxiety disorder, reach out for help today. Rachel Rabinor, LCSW is a psychotherapist in private practice; she helps women struggling with their transition to and through motherhood in her San Diego office. She also offers in-home counseling and Walk and Talk Therapy. For resources outside of San Diego, contact your local chapter of Postpartum Support International.
Spread the Word: Ask that New Mom About Her Mental Health #AskHer
When a woman is pregnant people are so eager to chat, engage and support her. Doors are held open by strangers. Family and friends gather to shower the expectant mother and her baby to be. Couples take babymoons to celebrate their time together as a couple and the new beginning that lies ahead. However, once baby is born, it’s not uncommon for mothers to be left behind while their new baby becomes the focus of attention— theirs and everyone else’s.
May is Maternal Mental Health Awareness Month worldwide, and today kicks off the May Campaign (May 2 - 6, 2016). The goal of the May Campaign is to increase knowledge about and awareness of the serious and devastating emotional complications that many women experience during pregnancy and after the birth of a child.
When a woman is pregnant people are so eager to chat, engage and support her. Doors are held open by strangers. Family and friends gather to shower the expectant mother and her baby to be. Couples take babymoons to celebrate their time together as a couple and the new beginning that lies ahead. However, once baby is born, it’s not uncommon for mothers to be left behind while their new baby becomes the focus of attention— theirs and everyone else’s.
This year the May Campaign is focusing on the importance of shifting the conversation from baby back to mom and encouraging you/me/us to #AskHer about her mental health. Ask the mothers you love and care for about: How are you sleeping? How are you eating? How are you feeling?
Why should you #AskHer?
You might be wondering why it's so important to ask her. One in seven women experience postpartum depression. There are many risks to both mom and baby if postpartum depression or anxiety goes untreated, including: a lower quality of life for mom, a decreased ability to function at home and at work, recurrent depression and suicide. Yes, suicide!
An infant with a mother whose depression goes untreated is at risk for an insecure attachment with their mother and delays in cognitive development. These are significant risks to both mom and baby.
But it doesn’t stop there. According to research, half of all men whose partners have postpartum depression are depressed themselves. Additional risks include a decrease in care of other children in the home and an increase in overall stress and discord within the family unit.
How to help a postpartum mom you’re worried about:
If you’re not sure if what she’s experiencing is part of the normal postpartum adjustment to motherhood or something more serious, this article can help you learn about 3 Differences Between Postpartum Depression and the Baby Blues. If you’re worried about her, below are three things you can do to provide support.
- Speak Up! Share your concern for her. Most struggling moms are relieved to hear there’s actually something wrong. Feeling so overwhelmed, it’s difficult to imagine how they’ll manage if what they’re experiencing is truly normal. This article here talks more about why it’s important for YOU to say something.
- Call her local chapter of Postpartum Support International. You can get her connected with the warmline, which can provide her with referrals to trained therapists and local support groups. There are even online groups if needed. If you can call with her, that’s even better.
- Be there for her. Listen to her. Hold her baby so she can shower, or rest. Make her food. Clean her house. Walk her dog. Fold her laundry. Listen.
At the end of the day, please don't forget to #AskHer. Ask the mothers you love and care for about their mental health: How are you sleeping? How are you eating? How are you feeling? If you suspect that you or someone you love is struggling with a perinatal mood or anxiety disorder, reach out for help. Rachel Rabinor, LCSW is a psychotherapist in private practice. She sees women struggling with their transition to and through motherhood in her private practice in San Diego. She also offers in-home counseling to help ease this transition See above for other San Diego and national resources.
How to #StartAsking for Support: The Journey of Secondary Infertility
You have a child, or maybe two or three. You want to grow your family but it's been 6 months or 12 and still nothing. Or you've gotten pregnant but have miscarried. Again, perhaps.
You discover on your own through your late night dates with google what you've got—Secondary infertility. No one's said it but that's what you've got.
This week is National Infertility Awareness Week (April 24-30, 2016) and the theme this year is “#StartAsking.” One of the goals of the #StartAsking campaign is to raise awareness, reduce the stigma and encourage people struggling to get the support they need.
While infertility itself is seldom discussed at dinner parties, secondary infertility is even more of a hush hush subject. Sharing your experience with secondary infertility can help invite those who love you to advocate for you and support your family during this challenging time.
What is Secondary Infertility?
You have a child, or maybe two or three. You want to grow your family but it's been 6 months or 12 and still nothing. Or you've gotten pregnant but have miscarried. Again, perhaps.
You discover on your own through your late night dates with google what you've got—secondary infertility. No one's said it but that's what you've got. According to Resolve, The National Infertility Association, secondary infertility:
is the inability to become pregnant, or to carry a pregnancy to term, following the birth of one or more biological children. The birth of the first child does not involve any assisted reproductive technologies or fertility medications.
Why hasn’t anyone mentioned it, you want to know? You wonder why your doctor shrugged you off and told you to keep trying. Are they ignorant? Optimistic? Lazy? What are they waiting for!?
There are so many complicated aspects to secondary infertility and coping with those who love you but who just don't get it. But the only way for them to know how hard it is and how lonely it is, is if we #StartAsking them to take a peek inside your world, to pay attention to your struggle, and understand what it’s like to experience secondary infertility.
Consider sharing this list with them as a way to help them understand what you’re going through. Tell them the number of the struggle listed below that's hardest for you today. Add your own. Let them in. Let them help you!
Common Struggles of Secondary Infertility
- You’re depressed and overwhelmed that you might not have another baby.
- You're mourning a loss. The loss of a baby. The loss of your dreams. Your life isn't going as planned and you have no control. You feel helpless.
- Your relationship is strained— it can be difficult to get on the same page about treatments and to connect on a deeper level outside of your timed TTC (trying to conceive) "appointments".
- The judgement— You feel judged in online communities and sometimes in the real world too because you have a child already and others don't. You wish you could tell them— there's enough sorrow to go around, folks!
- The appointments! Who has time for all the appointments (the other kinds!)? Your RE, OB, the HSG, the routine ultrasounds. Let's not forget your acupuncturist! All the work you need to miss or childcare you need to arrange. It's a LOT.
- You struggle with envy as those around you, unintentionally or not, become pregnant.
- Anniversaries hurt- your due date, when you had your (first/second/third) miscarriage, the holidays that coincide with those now infamous dates that are forever marred.
- The well meaning but unintended hurtful things your friends and family say in an effort to comfort you.
- Your child(ren). Yes- so lucky to have that source of light. but dealing with the emotional weight of repeat losses, the TWW (two week wait), negative tests... it's intense. If you'd like some suggestions on maintaining your bond with your child through this dark stage, you might find this article helpful.
- Your physical pain. The hormonal impact of infertility drugs- the anxiety, mood swings, weight gain. Or the nausea that comes with each hopeful pregnancy.
If you feeling inspired to #StartASking for support, consider sharing this article with someone you love who can help you through your journey.
If you’re struggling with primary or secondary infertility and think you could benefit from the support of a trained psychotherapist, reach out! In San Diego, call Rachel Rabinor, LCSW for a free 30 minute in-person consultation. She maintains a private practice in the Banker’s Hill neighborhood where she specializes in Maternal Mental Health including infertility and loss. Resolve is a great resource for those outside of San Diego.
3 Reasons to Try Walk and Talk Therapy
Walk and Talk Therapy is just that—walking while talking with a trained therapist. It’s exercise but not cardio. Collaborative and professional. Walk and Talk is a useful modality for many people. Anyone suffering from anxiety, depression, coping with grief or loss, or feeling stagnant in life may find it beneficial.
I just hung up the phone with a colleague who wanted to pick my brain about providing Walk and Talk Therapy. Our call got me thinking about all the incredible benefits of this, seemingly to some, out-of-the box therapy, and why more people should consider trying it.
Walk and Talk Therapy is just that—walking while talking with a trained therapist. It’s exercise but not cardio. Collaborative and professional. Walk and Talk is a useful type of treatment for many people. Anyone suffering from anxiety or depression, coping with grief or loss, or those feeling stagnant in life may find it beneficial. This article talks about the benefits for new moms and also talks more about what Walk and Talk is, and what it isn’t (How walk and Talk Will Change Your Life, Mama).
Here are three MORE reasons to consider Walk and Talk Therapy:
Walk and Talk Therapy allows you to take small steps towards your goals. It’s a great metaphor. With each step, you’re moving forward in life, leaving your problems behind figuratively and literally. You’re no longer thinking about starting therapy, you’re engaging in it actively. You’re no longer thinking about exercise, you’re moving. Small steps change lives.
- You’ll feel Better—Both therapy and exercise are linked to improved mood and a decrease in symptoms of depression and anxiety. Physical exercise releases endorphins, which naturally spark positive feelings that help to reduce levels of depression and anxiety and prevent depressive symptoms. Being in nature is not only restorative but can improve your positive outlook on life and your ability to cope and recover from stress and illness. Walk and Talk Therapy leaves many people with improved self-esteem and sleep, and a greater overall sense of well-being.
- Hello multi-tasking! Life is busy, and carving out time for exercise, fresh air and your mental health can be daunting. Combining movement and therapy in nature is a convenient way to make progress in multiple areas of life that need tending. We've all heard sitting referred to as the new smoking. It’s not enough to just think about our need for more exercise, we need tools and plans that allow us to implement exercise in ways that don’t add greater stress to our lives.
If you’ve been thinking about starting or resuming counseling, could Walk and Talk would be a good fit for you? What do you think? Please chime in below in the comments section!
If you’d like to learn more about Walk and Talk therapy and live in San Diego, schedule your free 30 minute in-person consultation to find out if I might be the right fit for you!
3 Differences Between Postpartum Depression and The Baby Blues
People often confuse the Baby Blues and Postpartum Depression. Some like to say that all moms have a bit of postpartum. Have you heard that? When I hear that I presume they're not sure what the difference is between the Baby Blues, which are normal mood fluctuations after having a baby, and something more serious like Postpartum Depression or Postpartum Anxiety.
People often confuse the Baby Blues and Postpartum Depression. Some like to say that all moms have a bit of "postpartum". Have you heard that? When I hear that I presume they're not sure what the difference is between the Baby Blues, which are normal mood fluctuations after having a baby, and something more serious like Postpartum Depression or Postpartum Anxiety (and then there's the very important fact that "postpartum" is actually a period of time, not a condition).
For the purpose of this post, I want to clarify that PPD and PPA are NOT the only mental health concerns during pregnancy or postpartum. They fall under the umbrella of Perinatal Mood and Anxiety Disorders (PMAD), but I wouldn't have caught your attention with that title now, right?
Are there visual cues to detecting Postpartum Depression?
It's not only regular folks who are confused about the differences, but some medical professionals are also a bit unclear. I've heard that some some professionals specializing in women's health don't formally screen for perinatal mood or anxiety disorders because they feel they can tell whether a mom is struggling with PPD just by looking at her. Is it possible, you wonder?
Here's a quick quiz: below are two images of postpartum women. Which woman has the Baby Blues? Which has Postpartum Depression? If you're struggling with Postpartum Depression right now, or have in the past you know better than to fall for this one: you don't have to be sad and teary to be diagnosed with a PMAD. In fact, many women make an enormous effort to look put together. If this sounds like you, you're definitely not alone.
Image A
image b
The Face of the Baby Blues
The massive hormonal shift immediately after birthing a baby will more likely have you looking like the image on the left, "Image A" than the one on the right, "Image B". A shocker for many despite the fact that the Baby Blues affects up to 80% of mothers and as I said earlier, are due to a normal fluctuation of hormones.
Danielle Haines, on the left (Image A), is a doula and midwife in-training. She posted this raw image of herself on Facebook a few months ago. It was taken days after giving birth to her son, and she shared it in an effort to shed light on what the adjustment to early motherhood really looks like. Sadly, there's still stigma attached to this normal postpartum experience. Women are unfortunately hesitant to share that motherhood isn't all ice cream and roses.
The Face of Postpartum Depression
The image on the right, of course, is Hayden Panettiere. She looks like so many new moms--walking on the beach, seemingly happy with her baby and fiancé. No visual cues that she is suffering. This is also how many women who are suffering survive, by projecting a put-together image of themselves, avoiding the shame and stigma that still persists. Meanwhile they're falling apart on the inside. Alone. Because they "look fine" no one pays attention. They slip through the cracks. Up to 20% of women experience a Perinatal Mood or Anxiety Disorder.
When this photograph of Panettiere was captured her baby was three months old. She sought treatment for postpartum depression seven months(!) after that image was publicized. Fortunately, times are changing and celebrities like Hayden Panettiere are more open about their real-life experiences adjusting to early motherhood. Thankfully there is a growing effort to destigmatize PMADs, and to motivate others to get the help they need.
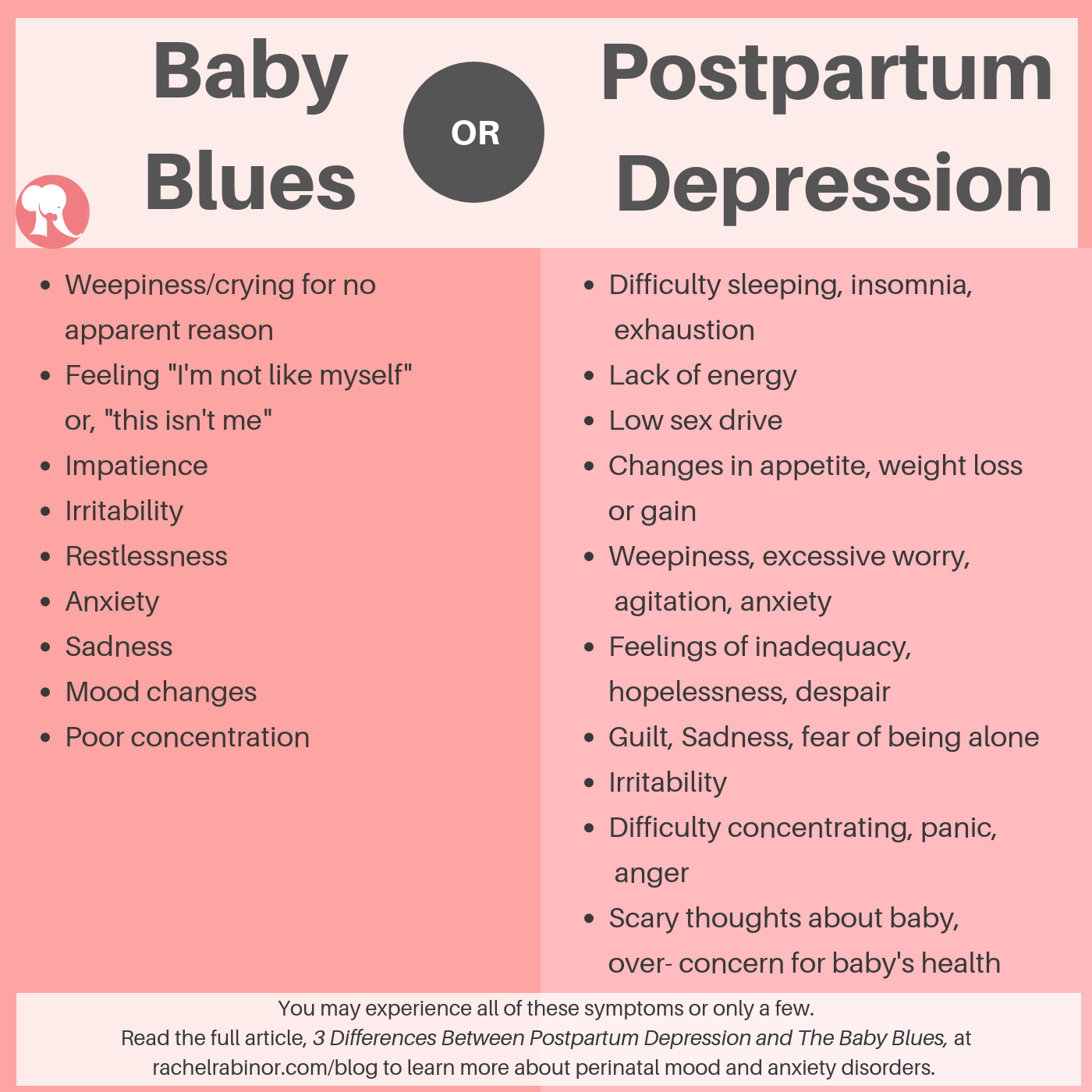
Symptoms of Postpartum Depression vs the Baby Blues
So if we (doctors included) can't tell by looking, how can we know if what we're feeling is part of the normal adjustment to early motherhood or something more serious? Below is a cheat sheet describing the different symptoms one may experience with either the Baby Blues or Postpartum Depression. You may notice some similarities. Keep reading below to better understand the differences.
It's not necessarily what you are feeling. It's how often you feel it, how long you have been feeling this way, and how much it impedes your functioning.
1-Duration
How long have you been feeling this way? The baby blues typically resolves within 2-3 weeks after giving birth, whereas Postpartum Depression symptoms continue for longer, and may present several weeks or months after having a new baby (*or bringing one home-- PPD impacts adoptive parents as well as fathers/non birthing parents).
2- Intensity
How much are these feelings interfering with your life? If you're not sure how to evaluate intensity, answer these questions:
Do I find it hard to care for my own basic needs or those of my baby or other children? Is my eating or sleeping affected by these feelings?
Are these feelings interfering with other important relationships? With my partner? Other family members? Friends? Work?
3-Frequency
How often are you feeling this way? Once a week? Once a day? Nonstop? There's a difference.
It's important to recognize that some of the most common symptoms of postpartum depression-- rage and anxiety for example-- look nothing like the stereotypical image of a saddened, depressed woman who can't get out of bed. Symptoms of the Baby Blues respond extremely well to rest and other forms of self-care. Here's an article that outlines 6 Ways to Improve your Postpartum Self-Care.
Getting help for Postpartum Depression
If you've been struggling with distressing thoughts and feelings for longer than two weeks, I recommend that you reach out to your doctor or a psychotherapist who specializes in perinatal mood and anxiety disorders.
And if it's less than two weeks but you just "know" something's not right, pay attention to that inner voice. Trust that you know yourself best and reach out for help. It really doesn't matter what we call it; you and your baby both deserve the care and attention you need to thrive. It's also important to reiterate that Postpartum Depression as referred to in this article, falls under the umbrella of perinatal mood and anxiety disorders, PMADs, which encompass other illnesses such as postpartum obsessive compulsive disorder, postpartum anxiety, postpartum post-traumatic stress disorder and postpartum psychosis.
If you or someone you know is struggling with a Perinatal Mood or Anxiety Disorder, please reach out for support. PMADs are very treatable. In my private practice in San Diego, California where I specialize in Maternal Mental Health, I offer a free 30 minute in-person consultation to find out if I'm the right therapist for you. Postpartum Support International (PSI) is a national organization that maintains a warmline and a list of trained providers specializing in Maternal Mental Health. If you’re in San Diego, CA, The Postpartum Health Alliance is our local chapter of PSI and a wonderful resource.
You Think Someone You Love Has PPD? Why YOU Need to Speak Up!
If you don’t speak up, the person you love might not get the help they need! Many women suffer in silence. Too many. More than 20 percent of moms are diagnosed with PPD; however, a recent study by BabyCenter shows that 40 percent do not seek medical help they need due to feelings of embarrassment, guilt and the expectation that they can get over it without professional help. There are many risks to mom and baby if postpartum depression or anxiety goes untreated, including:
Last week I got together with a new friend, Shelly, for a walk. When she learned more about the work I do with new and expecting mothers, the worry poured out of her. Shelly’s sister-in-law (SIL) had a baby 8 months ago, and she’s concerned about her. She's tired, irritable, incredibly anxious and doubting herself all the time (Yes, these are also symptoms of PPD--scroll to the bottom of this page for other symptoms you may not know about). Specializing in Maternal Mental Health, it’s par for the course to hear about sisters, friends, daughters and co-workers who are struggling with Postpartum Depression.
One in seven women deal with Perinatal Mood and Anxiety Disorders (PMADs), so really, it’s no surprise to hear about it so often. The thing that routinely does surprise me, however, is the hesitation many people share about approaching those they love with their concerns. This was Shelly to a T. She felt close to her SIL, but was apprehensive about recommending that she seek out some support.
Hesitant to offer support?
The more we talked the more I understood what was getting in Shelly’s way of reaching out. Shelly's the mom of a toddler and seems to have it together-- or together enough. She has a stable partner, family close by, a new business she’s passionate about; she’s confident and happy in her life. Her SIL, on the other hand, lives far from family and is further isolated by her husband’s current deployment with the Navy. She has a history of depression and other risk factors associated with PMADs.
By the end of our walk, I had a pretty clear grasp on Shelly’s hesitation to reach out to her SIL. She didn’t want her to feel judged, or less-than, by addressing concerns about her ability to cope with the adjustment to motherhood: A transition that has come fairly easily for Shelly. Shelly was also concerned about providing the right kind of support. With a history of depression, it was routine for family to jump in to “help” her SIL, and make everyday tasks easier. Her depression would subside for a bit and then the pattern would repeat. While a supportive family can be ideal in helping someone through their recovery, professional treatment may still be needed to address issues that may be contributing to the depression on a deeper level. Shelly wanted to help but she wasn’t sure how to do so effectively.
Why it’s important for YOU to speak up
If you don’t speak up, the person you love might not get the help they need! Many women suffer in silence. Too many. More than 20 percent of moms are diagnosed with PPD. However, a recent study by BabyCenter shows that 40 percent don't seek the medical help they need due to feelings of embarrassment, guilt and the expectation that they can get over it without professional help. There are many risks to mom and baby if postpartum depression or anxiety goes untreated.
RISKS OF NOT GETTING HELP WITH PPD
Risks to mom
- Lower quality of life
- Decreased ability to function at home or at work
- Risk of recurrent depression
- Suicide
Risks to baby
- Insecure attachment to mother
- Interference in cognitive development
Family stress and discord
Decreased care or neglect of other children
Loss of job/income
Also quite common is that women don’t even realize that what they’re experiencing isn’t normal! Just today I saw a third-time mom who started to recognize in my office that she had probably struggled with postpartum depression with her first two children without knowing. Sounds unbelievable but it’s true. The messages that women hear about motherhood reinforce that it’s natural, easy. That yes, you may be tired, but that’s normal. There’s a lot of grey area and it’s not always crystal clear whether what you’re experiencing is a normal adjustment to motherhood or something more serious. So if you notice something doesn’t seem right in someone you care about—Say something!
What to say to someone with Postpartum Depression
Shelly is a great example of someone who really wants to support someone they love, can identify their struggle, and for various reasons isn’t sure how to help. The reality is, it may not be the easiest conversation to have. But I find that women who are struggling are usually relieved to learn that there’s help available and that they don’t need to suffer in silence. Here’s a few suggestions of how to start the conversation:
1. Be direct
It’s important to be empathic, but it’s most important to be direct. Let her know that you’re worried about her; she doesn’t seem like herself. Let her know it’s normal, lots of women (1 in 7!) deal with PPD. It’s not uncommon for many women to go undiagnosed. Don’t let her slip through the cracks!
2. Be genuine
Speak from your heart. Let your love and care shine through. If she’s struggling to care for herself or her baby, this is serious. Remember, she’s not choosing to be neglectful, she’s struggling. You know she wants the best for her baby, for her family. Help her get the professional support she needs.
3. Be available
Make time for her. Once you connect her with people and resources she needs to improve her mental well-being, she will still need lots of support from people in her life who love her. She is vulnerable. Bring her food, go for a walk, watch her baby so she can take a shower. Keep her company.
If you or someone you know is struggling with a Perinatal Mood or Anxiety Disorder, please reach out for support. PMADs are very treatable. Postpartum Support International (PSI) is a national organization that maintains a warmline and also list of trained providers specializing in Maternal Mental Health. If you’re in San Diego, CA, The Postpartum Health Alliance is our local chapter of PSI and a wonderful resource.